Rethinking hyponatremia - a new framework for clinical practice
From a viewpoint of balance, the pathogenesis of hypotonic hyponatremia is remarkably simple: You can either
take in too much hypotonic fluid,
excrete too little of it in the urine
or a combination of both.
There really isn’t anything more to it (Box 1). Whatever fancy etiology of hyponatremia you are hearing about, the final common pathway is always: Too much drinking, too little peeing, or both.
To excrete relevant amounts of hypotonic urine, the kidneys have to
dilute the urine by reabsorbing more sodium and potassium than water,
maintain this dilution (For that, ADH-effects must be suppressed.)
and excrete high enough amounts of non-electrolyte solutes, generally urea (Box 2).
The hyponatremia menu
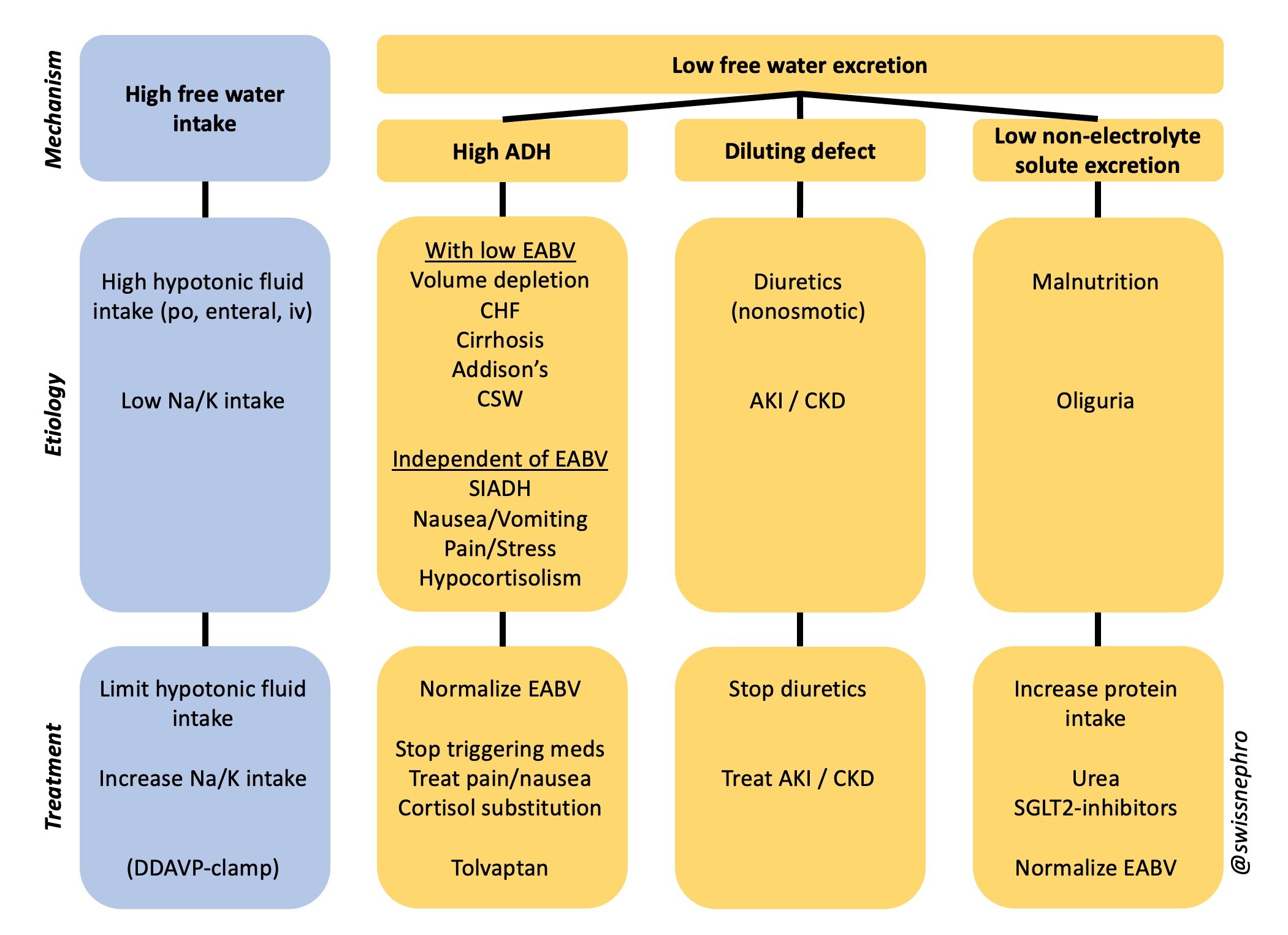
So, for clinical purposes one can distinguish four basic mechanisms of hyponatremia:
High free water intake
High ADH
Diluting defect
Low non-electrolyte solute excretion
All etiologies and therapeutic measures of hyponatremia can easily be integrated into this simple mechanistic framework:
The Hyponatremia Menu: Choose and combine all that applies!
Importantly, and I cannot stress this enough, these 4 categories do not exclude each other. In contrast to what current algorithms of hyponatremia generally imply, most hyponatremias are multifactorial and result from different combinations of these four basic mechanisms.
Combinations from within the different categories are perfectly possible as well: For example, hyponatremic patients with high ADH might have a low effective arterial blood volume AND a high ADH-condition that is independent of EABV as well.
The problem with current algorithms
Most current hyponatremia algorithms use a series of questions about urine osmolality, urine sodium concentration and/or volume status to distinguish different categories of hypotonic hyponatremia. The dichotomy (or trichotomy) of these algorithms has a number of significant drawbacks:
It wrongfully suggests that the different categories are mutually exclusive.
Branching points are reduced to simple either/or questions, ignoring the quantitatively continuous nature of the parameters in question.
Effective treatments often do not fit the diagnostic category.
So, instead of trying to determine the etiology of hyponatremia with a series of misleadingly dichotomous decisions, I recommend to check for the presence and extent of all four mechanisms and their respective etiologies in every patient with hyponatremia in parallel. Effective therapies for hyponatremia usually address different mechanisms as well.
Bottom Line
The graph above should be used like a menu from which to choose all components that match your individual patient with hyponatremia.
(How to assess the different mechanisms in clinical practice will be covered in another post.)
Addendum 06/2022
ADH-dependent and ADH-independent constraints on urinary dilution are not clearly distinguishable in clinical practice. I have thus simplified the above scheme: